Varicose Vein Treatments Available
Understanding Varicose Veins: Causes and Symptoms
Varicose veins are a common condition affecting many individuals worldwide. These enlarged, swollen veins often appear blue or dark purple and are most commonly found on the legs. The condition arises when the valves in the veins become weak or damaged, leading to blood pooling and vein enlargement. While often seen as a cosmetic issue, varicose veins can cause discomfort and lead to more severe health issues if left untreated.
Several factors contribute to the development of varicose veins, including:
- Age: As we age, veins can lose elasticity, causing them to stretch.
- Gender: Women are more likely to develop the condition, partly due to hormonal changes during pregnancy, pre-menstruation, or menopause.
- Family history: A family history of varicose veins increases the risk.
- Obesity: Excess weight puts additional pressure on the veins.
- Prolonged standing or sitting: Occupations that require long periods of standing or sitting can hinder blood flow.
Symptoms of varicose veins include aching or heavy legs, burning or throbbing sensations, muscle cramps, and swelling in the lower legs. In severe cases, the condition can lead to skin ulcers or blood clots, necessitating medical intervention.
Conservative Treatments: Lifestyle Changes and Home Remedies
Before considering more invasive procedures, many individuals find relief through conservative treatments and lifestyle adjustments. These approaches aim to improve blood circulation and alleviate symptoms, making daily life more comfortable.
Key lifestyle changes and home remedies include:
- Exercise: Regular physical activity, such as walking or cycling, helps improve blood circulation and reduce pressure on the veins.
- Weight management: Maintaining a healthy weight can alleviate pressure on the veins, reducing symptom severity.
- Elevation: Elevating the legs when resting can aid in blood flow and reduce swelling.
- Compression stockings: These specially designed stockings apply gentle pressure to the legs, supporting vein function and reducing discomfort.
- Dietary changes: A diet high in fiber and low in salt can prevent constipation and reduce swelling.
While these measures may not eliminate varicose veins, they can significantly alleviate symptoms and improve quality of life. It’s essential to consult with a healthcare provider to tailor these approaches to individual needs.
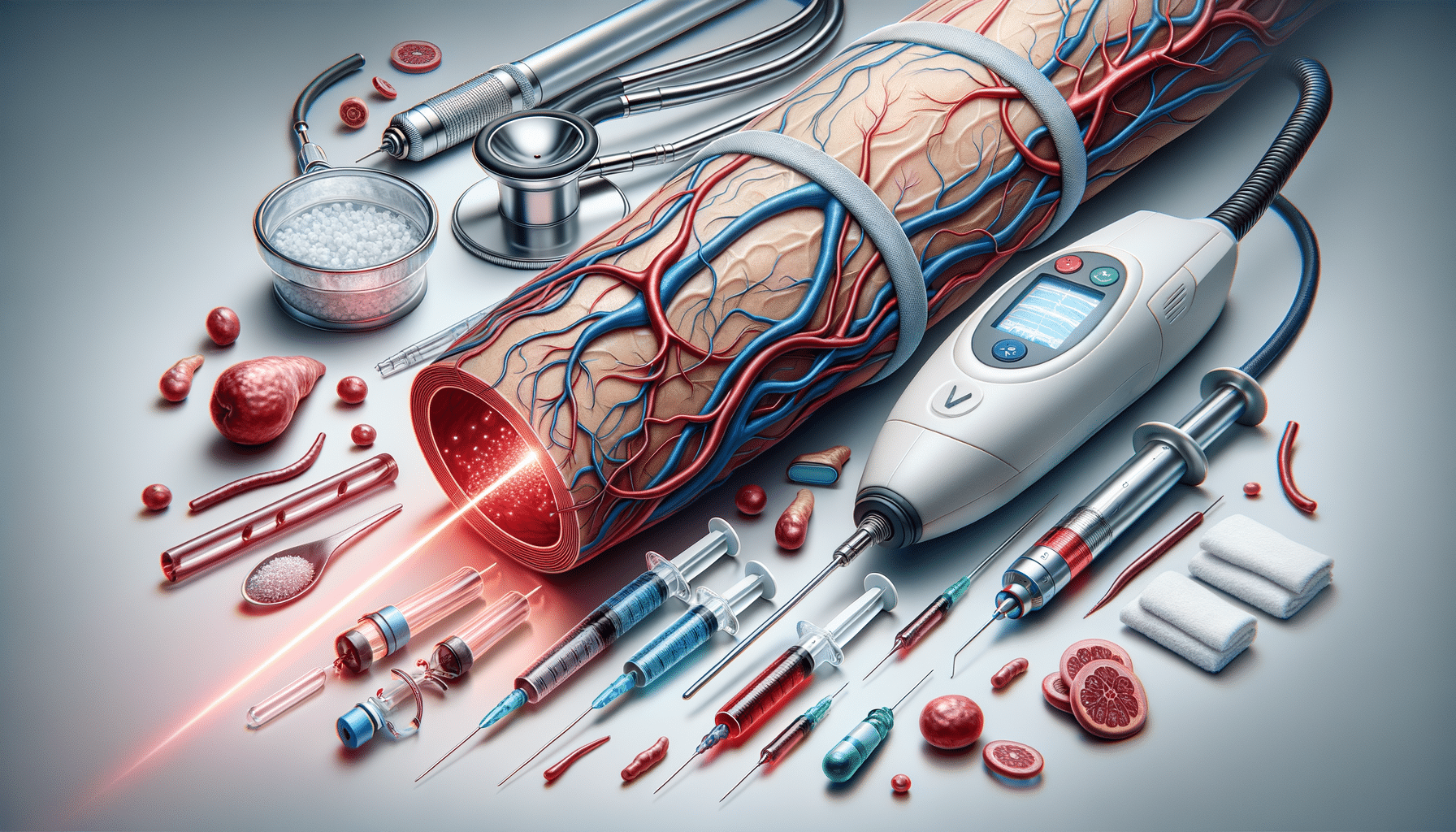
Medical Treatments: Minimally Invasive Options
For those seeking more definitive solutions, several minimally invasive medical treatments are available. These procedures are typically outpatient, involve minimal discomfort, and offer quick recovery times.
Popular minimally invasive treatments include:
- Sclerotherapy: This procedure involves injecting a solution into the affected veins, causing them to collapse and eventually fade. It’s effective for smaller varicose and spider veins.
- Laser treatment: Laser therapy uses strong bursts of light directed at the vein, causing it to slowly fade and disappear. This method is suitable for smaller veins.
- Endovenous laser therapy (EVLT): EVLT involves inserting a laser fiber into the vein, which heats and seals it. This treatment is effective for larger varicose veins.
- Radiofrequency ablation: Similar to EVLT, this technique uses radiofrequency energy to heat and close off the vein.
These treatments are generally safe and effective, with a low risk of complications. However, it’s crucial to discuss potential risks and benefits with a healthcare provider to determine the most suitable option.
Surgical Options: When to Consider Surgery
In cases where varicose veins are severe, or other treatments have failed, surgical intervention may be necessary. Surgery is typically reserved for large veins causing significant discomfort or health issues.
Common surgical procedures include:
- Vein stripping and ligation: This involves tying off and removing the affected veins through small incisions. It’s effective for severe cases but requires a longer recovery time.
- Ambulatory phlebectomy: This procedure involves removing smaller varicose veins through tiny skin punctures. It’s less invasive than traditional surgery and offers quicker recovery.
- Endoscopic vein surgery: Used for severe cases with skin ulcers, this technique involves inserting a small camera to visualize and remove the veins.
Surgical options are highly effective but come with risks associated with any surgical procedure. A thorough discussion with a vascular surgeon can help determine if surgery is the right choice.
Choosing the Right Treatment: Considerations and Consultations
Deciding on the appropriate treatment for varicose veins involves careful consideration of several factors, including the severity of the condition, personal preferences, and overall health. Consulting with a healthcare provider is crucial to making an informed decision.
Considerations when choosing a treatment include:
- Severity of symptoms: Mild symptoms may be managed with lifestyle changes, while more severe cases might require medical intervention.
- Personal comfort: Some individuals may prefer non-invasive treatments, while others are comfortable with surgical options.
- Cost and insurance coverage: It’s essential to consider the financial aspect and whether insurance covers the chosen treatment.
- Recovery time: Understanding the recovery process and time involved can influence the choice of treatment.
Ultimately, the decision should be made in collaboration with a healthcare provider, ensuring that the chosen treatment aligns with personal goals and medical needs.