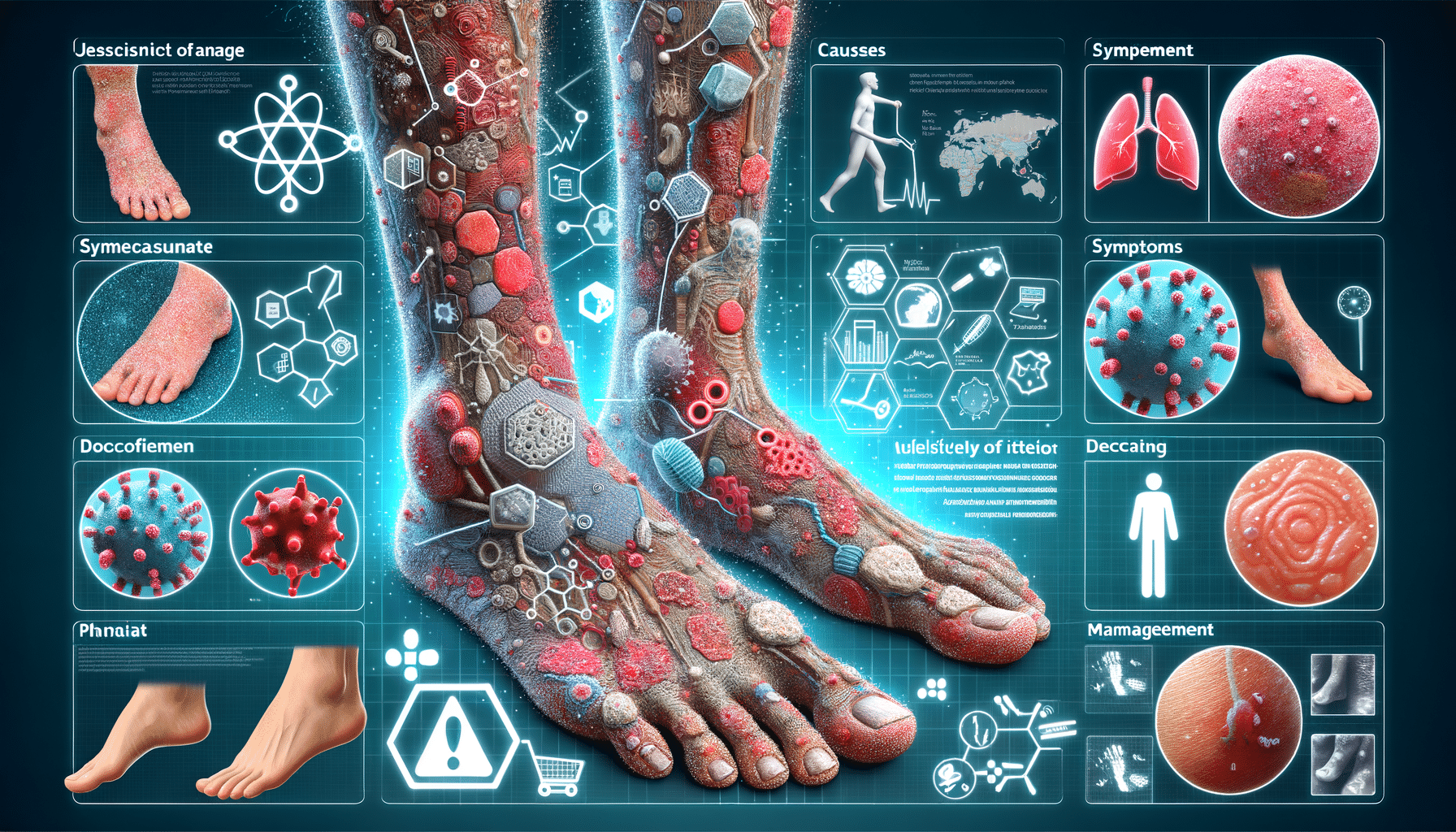
Understanding Feet Psoriasis: Causes, Symptoms, and Management
Introduction to Feet Psoriasis
Psoriasis is a chronic skin condition that affects millions worldwide, and when it targets the feet, it presents unique challenges. Feet psoriasis is not only physically uncomfortable but can also impact daily activities due to the constant use of our feet. Understanding this condition is crucial for effective management and improving quality of life.
Feet psoriasis can manifest as red, scaly patches on the soles and toes, often accompanied by itching and pain. The skin may become thick and cracked, making walking or standing for extended periods difficult. This article delves into the causes, symptoms, and management strategies for feet psoriasis, offering insights into this often-overlooked condition.
Causes and Risk Factors of Feet Psoriasis
The exact cause of psoriasis, including feet psoriasis, remains unclear, but it is believed to be an immune system disorder. In this condition, skin cells multiply at an accelerated rate, leading to the buildup of scales and red patches. Several factors can trigger or exacerbate feet psoriasis:
- Genetics: A family history of psoriasis increases the likelihood of developing the condition.
- Stress: Emotional stress can trigger or worsen psoriasis symptoms.
- Infections: Certain infections, such as strep throat, can trigger psoriasis flare-ups.
- Injury to the Skin: Cuts, scrapes, or other skin injuries can trigger a psoriasis outbreak on the feet.
- Weather: Cold, dry weather can worsen psoriasis symptoms.
Understanding these triggers can help in managing feet psoriasis more effectively, allowing individuals to take preventive measures and reduce the frequency of flare-ups.
Recognizing Symptoms of Feet Psoriasis
Identifying feet psoriasis is essential for timely intervention. The symptoms can vary in severity and may include:
- Red Patches: These are often covered with silvery scales and can be itchy or painful.
- Thickened Skin: The skin on the feet may become thick and hard, leading to discomfort.
- Cracks and Bleeding: Severe cases may result in cracks that bleed, increasing the risk of infection.
- Swelling and Stiffness: The joints in the feet may become swollen and stiff, affecting mobility.
It’s crucial to differentiate these symptoms from other foot conditions, such as athlete’s foot or eczema, to ensure appropriate treatment. Consulting a healthcare professional for an accurate diagnosis is recommended.
Effective Management Strategies for Feet Psoriasis
Managing feet psoriasis requires a comprehensive approach that includes both medical and lifestyle interventions. Here are some strategies that can help:
- Topical Treatments: Creams and ointments containing corticosteroids or vitamin D analogs can reduce inflammation and scaling.
- Phototherapy: Exposure to ultraviolet light under medical supervision can help slow down skin cell production.
- Moisturizers: Regular use of emollients can keep the skin hydrated and reduce cracking.
- Foot Care: Wearing comfortable shoes and using foot pads can alleviate pressure on affected areas.
- Stress Management: Techniques such as yoga or meditation can help reduce stress levels, potentially minimizing flare-ups.
It’s essential to work closely with a healthcare provider to tailor a treatment plan that suits individual needs and lifestyle.
Conclusion: Navigating Life with Feet Psoriasis
Living with feet psoriasis can be challenging, but with the right knowledge and strategies, it is possible to manage the condition effectively. Recognizing triggers, understanding symptoms, and adhering to a comprehensive treatment plan can significantly improve one’s quality of life. As research continues to advance, there is hope for more effective treatments and, ultimately, a better understanding of this chronic condition. Whether you’re newly diagnosed or have been managing feet psoriasis for years, staying informed and proactive is key to navigating this journey.